Abstract
Autoimmune hemolytic anemia (AIHA) is a rare disease due to autoantibodies directed against erythrocyte epitopes. The clinical course is greatly heterogeneous with different anemia severity at onset, occurrence of relapses and AIHA-related complications. The latter include thrombosis and infections that represent major causes of morbidity and mortality in this patient population. Predictors of such complications and preventive measures are object of active investigation.
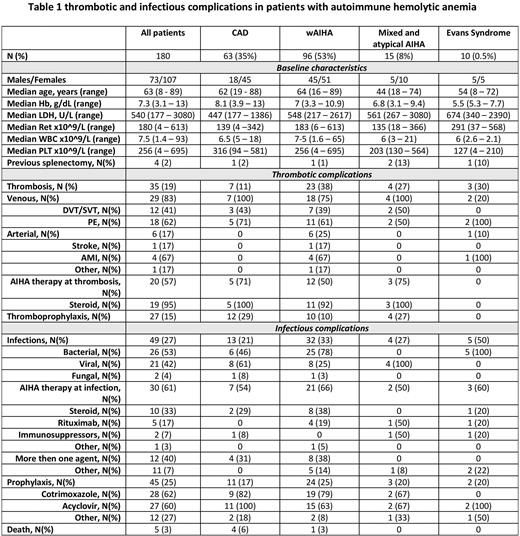
In this observational retrospective study the occurrence of infections and thrombosis was evaluated among 180 AIHA patients from 9 Italian hematologic centers. Events' severity was graded according to CTCAE and association with AIHA type, hematologic parameters and therapies was analyzed. Anti-thrombotic and anti-infectious prophylaxis were also collected.
As shown in table 1, patients were mainly middle aged females, AIHA type was consistent with known epidemiology (53% warm, wAIHA; 35% cold, cAIHA; 8% mixed and atypical cases), and 10 patients suffered from Evans syndrome (ES, association of AIHA with immune thrombocytopenia/neutropenia).
Thrombotic events occurred in 35 cases (19%), mainly in wAIHA and mixed/atypical cases (25 versus 11%, p=0.02), and more often interested the venous district (83%) and were grade 3 pulmonary embolism in 62% of cases. Arterial episodes were rare but mainly grade 4 and included 4 myocardial infractions, 1 stroke, and 1 retinal artery occlusion. All arterial episodes occurred in wAIHA patients (p=0.02). Notably, nearly all patients were on active steroid treatment at the time of thrombosis, likely related to active hemolysis. Among the 4 previously splenectomized patients 3 experienced thrombosis. No relationship were noted with baseline hematologic values. Interestingly, only 15% of cases had received primary thromboprophylaxis mainly with low molecular weight heparin, and none of them experienced thrombosis.
Regarding infections, 49 grade >2 events (27%) were registered mainly bacterial or viral, and rarely fungal. Five grade 4 and 1 fatal SARS-CoV-2 pneumonia. At the time of infection, 2/3 of patients were on active AIHA treatment either with steroids (33%) or rituximab (17%), and 40% with more than 1 agent. No statistically significant associations were noted among infections and AIHA type, baseline hematologic values, ongoing therapy, nor previous splenectomy, but for a higher trend of events among ES patients. Cotrimoxazole and acyclovir prophylaxis had been administered in one fourth of cases, mainly upon rituximab treatment or use of cytotoxic immunosuppressors.
In conclusion, these data confirm a remarkable prevalence of thrombotic and infectious complications in AIHA patients and suggest that current prophylactic measures, performed in a small fraction of cases only, should be implemented. Interestingly, thrombotic episodes were mainly high grade and more frequent in patients with wAIHA and mixed/atypical cases, usually showing more severe anemia at onset; the association with active steroid treatment suggests a link to active hemolysis as a risk factor for thrombosis. Although no predictors of infections emerged, the association with previous therapy lines more than with actual AIHA treatment deserves further investigation.
Disclosures
Fattizzo:Momenta: Consultancy; Amgen: Consultancy; Sobi: Speakers Bureau; Novartis: Consultancy, Speakers Bureau; Alexion: Consultancy, Speakers Bureau; Janssen: Consultancy. Barcellini:Novartis: Honoraria; Bioverativ: Membership on an entity's Board of Directors or advisory committees; Biocryst: Honoraria; Apellis: Honoraria; Incyte: Membership on an entity's Board of Directors or advisory committees; Momenta: Honoraria; Janssen: Honoraria; Alexion: Honoraria; SOBI: Honoraria; Agios: Honoraria, Research Funding; Sanofi: Honoraria, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal